

Pregnancy is a time of incredible change. Your body is shifting rapidly to grow and sustain new life, and with that comes a wide range of physical sensations.
Unfortunately, some of those sensations involve discomfort.
Many pregnancy discomforts are so common that we’ve begun to think of them as “normal” or “inevitable.” But the truth is, though certain types of discomfort are expected, most point to underlying issues we can address with real solutions.
In other words, you don’t have to resign yourself to suffering just because you’re pregnant.
With this in mind, let’s walk through some of the most common discomforts during pregnancy, their root causes, and what we suggest for each.
Common, Not ‘Normal’: 7 Pregnancy Discomforts
At Haven, we often hear about a familiar group of symptoms: heartburn, constipation, sleep troubles, fatigue, leg cramps, back and pelvic pain, and urinary leakage.
While common in pregnancy, these pains usually stem from underlying issues and have — thankfully — some relatively simple solutions.
1. Heartburn and Indigestion: A Perfect Storm
One of the most frustrating (and infamous) pregnancy discomforts is heartburn, which results from a perfect storm of factors. As your body produces more progesterone, digestion slows and the sphincter between your esophagus and stomach relaxes. At the same time, your growing belly puts pressure on your abdomen, pushing stomach contents upward.
There’s also a thought that stomach acid may decrease during pregnancy, which, perhaps counterintuitively, could also contribute to heartburn.
What You Can Do About Heartburn
Since heartburn causes vary and everyone’s body differs, you may have to try a few approaches to see which solutions work for you.
For prevention, here are a few simple approaches you can start with:
- Eat smaller, more frequent meals to avoid overloading your stomach.
- Stay upright after eating so gravity helps your stomach contents stay where they belong.
- Take digestive enzymes before meals to improve digestion.
- Drink diluted apple cider vinegar (1 tablespoon in 1 cup of water) before meals to improve digestion. If you struggle with the taste, mixing in a flavored electrolyte powder can help (we carry some great options in our office!).
- Avoid common trigger foods like fried or spicy foods, chocolate, tomatoes, caffeine, and (for some) mint.
- Take a 10–15 minute walk after bigger meals to aid digestion.
If you need to stop heartburn once it’s started, you can try natural treatments like:
- Eating ****a handful of raw almonds
- Taking papaya enzymes
- Drinking a ¼ tsp. of baking soda mixed with a little water (use sparingly)
Constipation: The Big Slow Down
Constipation is especially common in the first trimester when progesterone is high. This hormone quiets your whole body, an essential function that helps your uterus receive and nurture your baby. However, it also slows your digestive system — everything from your mouth to your colon — which frequently leads to constipation.
What You Can Do About Constipation
- Increase fiber in your diet.
- Drink 100 ounces of fluids daily, with at least 32 ounces containing electrolytes.
- Take 400–800 mg magnesium glycinate, starting low and increasing until you begin to notice loose stools, then backing off.
- Incorporate a raw carrot salad with coconut oil, salt, pepper, and apple cider vinegar into your diet.
- Increase vitamin C by 1,000 mg daily.
- Add flax seeds to smoothies or sprinkle on salads.
- Eat 2–3 dates or prunes daily.
Addressing constipation has the additional advantage of preventing or improving another common pregnancy pain — hemorrhoids — as well.
Trouble Sleeping: More Than Discomfort
Trouble falling or staying asleep is a very common pregnancy “pain,” especially in the first and third trimesters. Hormonal shifts, a growing belly, and the need to pee more often can all make sleep difficult. Low blood sugar in the middle of the night and increased nighttime metabolic activity can also play a role.
What You Can Do About Sleep Issues
I often encourage clients to establish good sleep hygiene habits to help them fall asleep more effectively. This includes adjustments like:
- Putting away screens and blue light 2 hours before bed (if you like to read at night, opt for a paper book instead)
- Dimming the lights
- Limiting fluids right before sleep
- Taking a warm Epsom salt bath
- Keeping a journal by your bed so you can “brain dump” racing thoughts onto the pages before sleeping or if you wake in the middle of the night
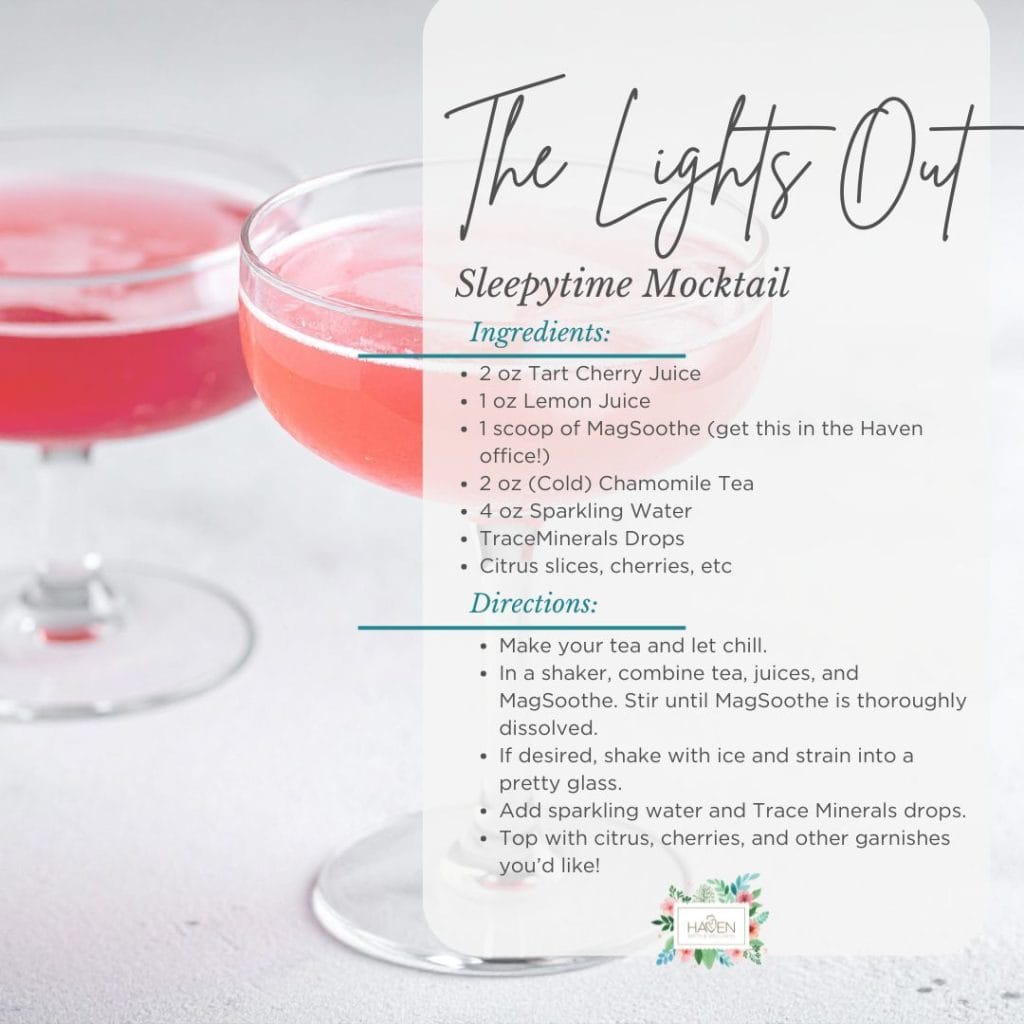
Some women find drinking tart cherry juice, which is naturally high in melatonin, helpful right before bed. You can even make it a mocktail! We have a recipe suggestion below to get you started, but feel free to make it your own.
To help prevent blood sugar dips from waking you at 3 a.m., you can try a fat- and protein-rich snack, like a handful of pistachios (another high-melatonin food). Snacks like this also help you fall back to sleep if you wake up in the middle of the night.
Fatigue: When Your Body Needs More
Pregnancy places massive demands on your body. You’re growing a whole person, and that requires energy and resources. It makes sense you’d need more rest, especially during a growth spurt!
Besides poor sleep, fatigue can stem from a host of sources, including dehydration, not eating enough, low blood sugar, thyroid issues, and iron or B12 deficiencies.
What You Can Do About Fatigue
- Talk to your provider so they can run labs to rule out deficiencies.
- Do a dietary recall for the past 4 or 5 days to ensure you’re getting 80–100 g. protein and 100 oz. fluid daily.
- Give yourself permission to nap and rest when needed.
- Try NORA tea, which includes nettles, oat straw, red raspberry leaf, and alfalfa, to boost your mineral intake.
- Consider adding Trace Minerals to your water to restore other essential nutrients.
Most women are undernourished without realizing it — especially if little ones are eating half of what’s on their plates! Make sure you’re getting all the fuel your body needs to do its incredible work.

Leg Cramps: A Deficiency Signal
Leg cramps during pregnancy are often a sign of magnesium deficiency. Magnesium gets used up quickly during times of stress, and it’s incredibly important during pregnancy.
What You Can Do About Leg Cramps
Besides encouraging intentional, daily movement like walking and stretching, we usually recommend that our clients supplement with magnesium throughout their pregnancies. You can absorb magnesium in multiple forms, including:
- Oral supplements like [MagSRT](https://www.jigsawhealth.com/products/best-magnesium-magsrt?) tablets (malate) or [MagSoothe](https://www.jigsawhealth.com/products/magsoothe-magnesium-glycinate?) powder (glycinate), both of which we carry in our office
- **Epsom salt baths**
- Magnesium oils or creams applied to the legs and feet (we carry one we love here in the office)
Back and Pelvic Pain: Signs of Deeper Dysfunction
Back and pelvic pain often show up as your body accommodates the rapidly growing weight and size of your uterus. But this pregnancy pain isn’t something you just have to accept. It’s usually a sign of muscular, joint, or ligament dysfunction, and I frequently see it tied to pelvic floor weakness.
Common symptoms of pelvic floor weakness include a sensation of pelvic pressure, feeling like your baby is going to “fall out,” or experiencing urinary leakage.
What You Can Do About Back and Pelvic Pain
You don’t have to wait until after birth to strengthen your body. In fact, I encourage you not to (though always speak with your provider first). Start working to strengthen your pelvic floor and surrounding muscles by:
- Seeing a chiropractor for alignment support
- Exploring physical therapy for targeted strengthening
- Starting pelvic floor PT for specialized care
Strengthening your body — especially your pelvic floor — right now can lead to a more comfortable pregnancy and a better postpartum recovery.
Urinary Leakage: Another Sign of Weakness
Urinary leakage is another pregnancy pain that’s so common we often think it’s unavoidable. But urinary leakage is usually just another sign of pelvic floor weakness, and there’s a lot we can do to support your body.
What You Can Do About Urinary Leakage
- Seek pelvic floor PT for specialized exercises.
- Focus on squats more than Kegels.
- Incorporate bodywork throughout pregnancy to support alignment and muscle balance.
Pregnancy Discomfort: Small Changes, Big Relief
Pregnancy is a state of wellness, so wellness-promoting practices can help you feel more comfortable, even if they aren’t targeted toward the specific pregnancy discomforts in this post.
By focusing on what you can control — how much you eat and drink, how often you move your body, how well you sleep, and how you manage stress — you give your body the support it needs and make a real difference in how you feel.
Final Thoughts on Discomfort in Pregnancy
Most women experience discomfort during pregnancy to some degree, but you don’t have to accept it as part of the package. Reaching out for support and exploring solutions isn’t dramatic or high-maintenance — it’s taking care of yourself and your growing baby.
So, don’t settle for the idea that pregnancy has to be miserable. You should never feel bad for asking questions about your symptoms or comfort. Bring up your pregnancy pains with your provider so that, together, you can seek ways to optimize your well-being.

Lauren Drees is a Certified Nurse Midwife and the founder of Haven Birth and Wellness. With over a decade of experience and having attended more than 1,000 births, Lauren is dedicated to providing compassionate, personalized care to women throughout their pregnancy, birth, and beyond.
